|
Getting your Trinity Audio player ready...
|
In the past, an imperfect and often complicated health care system, along with rising costs, impacted consumers’ ability to easily access care.
In fact, nearly 11% of adults nationally and nearly 13% in Florida avoided care due to the expense in the previous year, according to the America’s Health Rankings 2024 Annual Report.
As technology continues to reshape many aspects of our lives, employers and health plans are increasingly offering new digital tools, benefits, and programs that aim to make the health care experience simpler, more affordable, and better.
Here are three tips to more easily connect with quality care and potentially save more money.
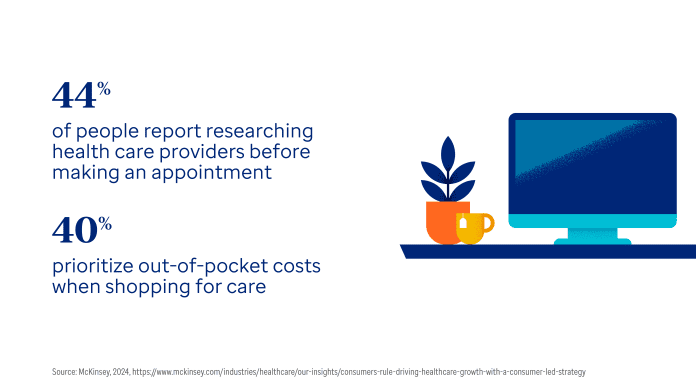
Take advantage of digital tools that help you compare care options: Many people like to research products before making a purchase, and the same is often true when it comes to health care. In fact, a recent study found that nearly half of people research doctors before scheduling an appointment.
Comparing care options ahead of time and making more informed decisions may result in better access to care and lower costs. Some employers and health plans now offer innovative solutions that aim to do just that.
Some of these new digital tools provide personalized results through a mobile app and website that help people make more informed decisions — like UnitedHealthcare’s new Smart Choice provider search experience.
This enhanced provider search experience creates a clear and straightforward approach to navigating care options by showing eligible members prioritized Smart Choice results with a dynamic score for each provider based on quality, convenience and the member’s health benefits and personal preferences.
Eligible UnitedHealthcare members with employer-sponsored health plans now have access to Smart Choice through the member app and website. Talk to your employer and health plan about what’s available to you.
Understand what wellness programs are available. About 80% of U.S. businesses with more than 50 employees now offer wellness programs, according to a recent survey, but many people don’t fully take advantage of all that’s available to support their health and well-being.
Some employer wellness programs can help people stay focused on their health goals, manage chronic conditions like type 2 diabetes and obesity, and even save more money, in part by utilizing technology.
UnitedHealthcare’s Level2® combines the technology of a continuous glucose monitor (CGM), easy-to-use member mobile app and a virtual care team of doctors, nurses, registered dietitians and a coach. Level2 aims to help people living with type 2 diabetes gain valuable insights to help improve their glucose levels.
You may be eligible for incentive-based wellness programs available through some employers designed to reward healthier choices. With these programs, eligible members can earn rewards for completing tasks like taking a health survey, getting an annual checkup, walking a certain number of steps, tracking hours slept and more.
Make your mental health a priority. Taking care of your mental health is important to your overall well-being as your emotional frame of mind may impact your physical health. If you’re struggling, treatment may help you feel better and live a healthier life.
Mental health challenges continue to grow and can have a significant impact on working age adults and many others. To focus on just one condition, 40 million American adults suffer from anxiety disorders that can impact quality of life and well-being, and anxiety is now the No. 1 mental health issue among American workers.
To address these challenges, many employers offer accessible and flexible mental health offerings — such as therapy apps and virtual counseling, which can provide convenient, confidential support.
One example is Calm Health. It’s an evidence-based mental health app that provides personalized support to help users manage their well-being. Calm Health offers resources to help support in-the-moment mental health, including:
- Mental health screenings
- Coaching and therapy referrals
- Personalized programs and daily self-care content.
Some health plans also offer behavioral health care programs to help with substance use, stress, anxiety, depression and more. Some health insurers also have specially trained advocates available to help members find the right type of behavioral health care or resources.
Make virtual care a starting point. Virtual care, also called telehealth, has expanded from helping people who are already sick to detecting and preventing illnesses and more effectively managing chronic conditions.
Many people enjoy the flexibility offered by virtual care, and some plans are now built around it. Virtual care offers 24/7 access to urgent care, in addition to access to medical and behavioral health and other care via a smartphone, tablet or computer — and transitions to in-person support, when necessary. Other options may include virtual primary care for regular health visits or virtual therapy for care from a behavioral health professional.